Stories
World’s first valve replacement procedure using Extended Reality
System “brings OR” to remotely located specialist for virtual support
Extended reality (XR) is typically associated with entertainment because of its immersive qualities. However, XR made a world first in healthcare when it was recently used to bring the operating room to a specialist located 500 kms away. This included the use of a holographic step by step clinical pathway developed in Canada.
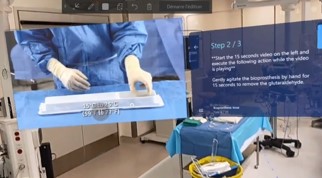
Using a co-developed system integrating the Microsoft HoloLens2 headset, a team of cardiac specialists at the Jewish General Hospital (JGH) in Montreal carried out a transcatheter valve implantation (TAVI), led by a training specialist located in Toronto. Wearing the XR headset, the performing surgeon was able to see a step by step 3D rendering of the clinical pathway overlaid in his visual field as he worked, while a TAVI specialist monitored and advised in real time from Toronto.
For the surgeons, the experience is like having the training specialist next to them in the OR, with the added benefit of not having to look up at various screens during the procedure. Meanwhile, the remotely located specialist or proctor, can access the patient’s vital details and see exactly what the practicing surgeon sees in real time -- an experience that is unique to this project.
“Everybody who uses this technology is blown away by it,” says Dr. Emmanuel Moss, Chief of Cardiac Surgery at the JGH. “It feels like you really have an expert standing right next to you and helping you do your best for the patient.”
When training surgeons on a new procedure, the established surgical specialist typically travels to other hospitals to supervise and train new specialists. This means coordinating schedules, including flights, hotels and other logistics – a challenge even without a global pandemic.
The success of this XR project could mean savings to hospital resources and may reduce barriers to patient care by facilitating training of innovative medical procedures.
The success of this XR project could mean savings to hospital resources and may reduce barriers to patient care.
At the start of the pandemic, the Jewish General Hospital in Montreal looked at virtual reality technology to help protect staff and patients by limiting physical exposure, as well as reducing the need for resources like PPE.
The success of the pilot project using the HoloLens system led to the development of the remote TAVI initiative. When JGH wanted to expand the project, Medtronic stepped up with its minimally invasive TAVI pathway, and engineering firm Auger Group Conseil (AGC) applied their Microsoft platform expertise. AGC was able to put voice, image, and other vital monitoring together with minimal lag to facilitate the experience for both the practicing specialist and the remotely located proctor.

Minimally invasive procedures such as TAVI are already helping to significantly improve patient recovery times compared to traditional procedures.
Reduced length of stay is a critical factor that can allow hospitals to recover their backlog of elective surgeries that may have been postponed during pandemic peaks. Enabling more specialists to learn innovative procedures further assists in optimizing hospital capacity, a vital component to recovery, and one that will have long term benefits overall.
“We started with TAVI because of the urgency for cardiac cases,” says Richard Paré, regional director of Cardiac portfolio at Medtronic Canada, “However, the XR pathway can be extended to many other existing procedures, now that we have proven the reliability and security of the system.”
Collaborations such as this are part of the Medtronic legacy. Co-founder Earl Bakken grew the company from a start-up in his garage through collaboration with a Minnesota hospital that was looking for a solution to bulky AC-powered pacemakers. This led to the first portable battery-operated pacemaker created by Bakken in the 1950s. At the time, this innovation helped save lives that were at risk due to power failures.
Reduced length of stay is a critical factor that can allow hospitals to recover their backlog of elective surgeries that may have been postponed during pandemic peaks.
Today’s collaboration operates under the same spirit of innovation — the lasting impact of this initiative is what drives bold ideas for the benefit of patients everywhere.