Stories
New research finds better patient outcomes and reduced costs for patients on ventilators
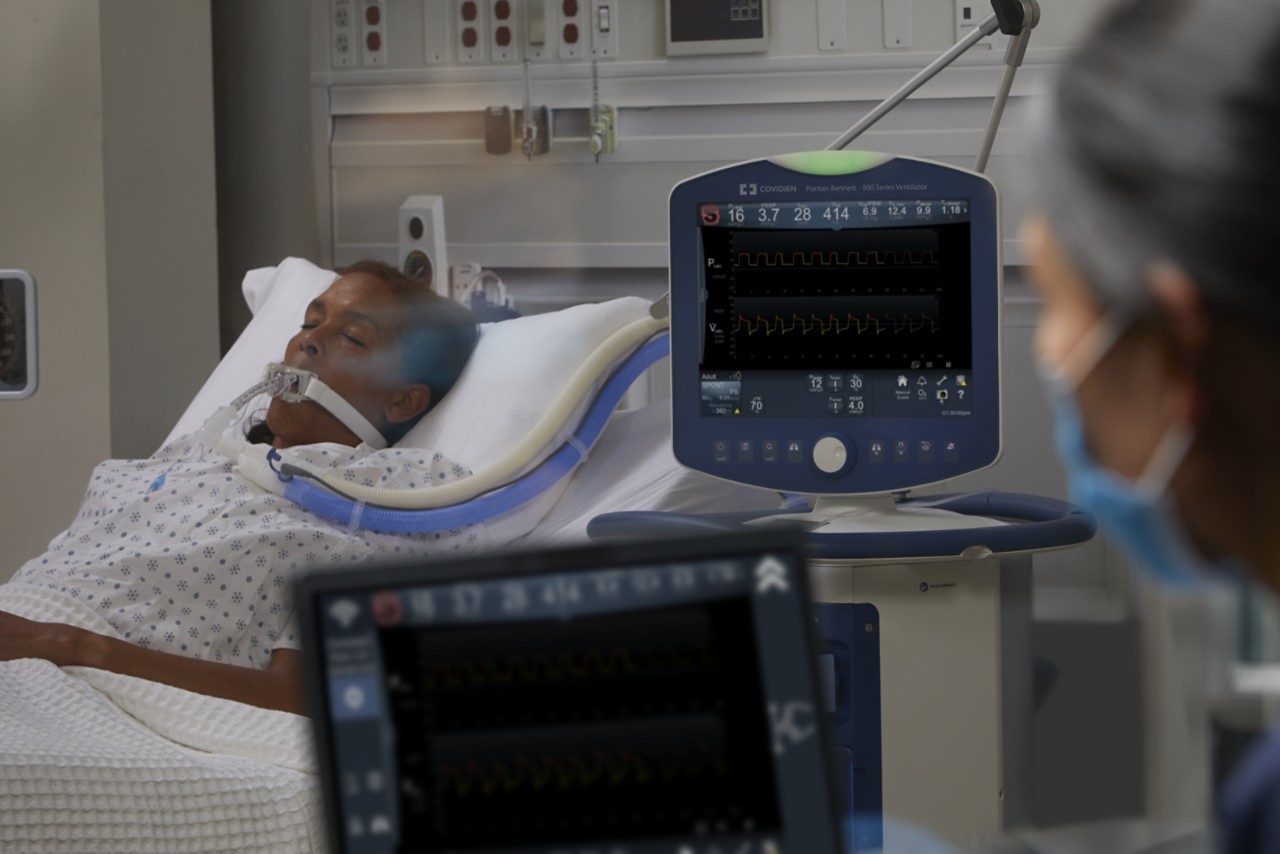
The COVID-19 pandemic shed greater light on the importance of Canadian hospitals ensuring they have adequate resources and staffing in place to provide ventilation to critically ill patients who need assistance breathing.
Intensive care units at hospitals across the country were forced to scramble to add beds, medical staff and ventilators to keep up with surging demand, particularly during the earlier waves of the pandemic.
Now, as the pandemic continues to simmer and they try to best manage strained budgets amid a health human resources crisis, hospitals and their government funding partners may be asking themselves what kind of ventilation is most cost-effective and delivers the best outcomes for patients?
A recently released Canadian research paper – Proportional-Assist Ventilation with Load-Adjustable Gain Factors for Mechanical Ventilation: A Cost-Utility Analysis – provides food for thought.
The study synthesized available evidence from previous research to explore the cost-utility of two methods of ventilation used in Canada – pressure support ventilation (PSV), a form of mechanical ventilation in which each breath is supported by a constant pressure set by a clinician, and proportional assist ventilation (PAV), in which the ventilator’s software adjusts the level of assistance to match the activity of a patient’s respiratory effort.
It found that PAV is more cost-effective, delivering a savings of $7,642 per patient, compared to PSV. At the same time, PAV also benefited patient care, increasing a measurement of quality of life by 16 per cent.
“Mechanical ventilation plays an important role in critical care and there will likely always be a need for it to some extent in Canadian ICUs, but based on all of the data we collected and analyzed, it’s likely that Canadian hospitals will find PAV to be more cost-effective than conventional ventilation support for Canadian hospitals and lead to more positive outcomes for patients,” says study co-author Rhodri Saunders.
Respiratory Therapist Danny Veniott says the study provides further confirmation for what he sees firsthand on a daily basis in his role as Program Manager of the Respiratory Therapy and Airways Clinics at St. Mary’s General Hospital in Kitchener.
“Our own data shows us we’re able to get more people off the ventilator and able to do it much more quickly when we use our PAV protocol, than with other modes of ventilation, including PSV,” he says.
St. Mary’s began using PAV as its predominant form of ventilation nearly a decade ago after a pilot project convinced leadership of the patient benefits, including less ventilation time, quicker recovery, fewer negative side effects and reduced reliance on sedatives and medications. The hospital treats approximately 1,300 patients per year who require ventilation, including those with chronic obstructive pulmonary disorder, multi-system failure and acute cardiac issues.
“We’ll use traditional full-support modes when a patient is acutely ill, but as soon as they’re stable enough to breathe spontaneously with assisted ventilation, then we get them on PAV,” says Veniott.
Richard Kauc, a Respiratory Therapist and Ventilation Specialist at Medtronic Canada, is hopeful the study may provide more hospitals the data they need to offer patients greater access to PAV. Medtronic manufactures critical care ventilators with PAV for the global market.
“The true merits of PAV should be seen in the quality outcomes – less time on a ventilator, less time in the ICU and less likely to die,” he says. “This study looked at existing research that shows better patient outcomes and wanted to see of there was also an economic benefit, and the answer was, ‘Yes.’”
A full version of Proportional-Assist Ventilation with Load-Adjustable Gain Factors for Mechanical Ventilation: A Cost-Utility Analysis can be found here.
Reprinted, courtesy of Hospital News