Stories
Patient-first vision at NBHC leads to optimizing funding models for minimally invasive TAVI procedure
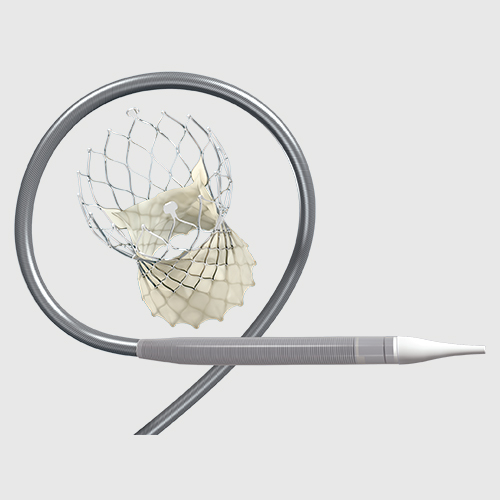
Approximately 20% of Canadians will experience aortic stenosis (AS) once they reach the age of 65. For those with severe AS requiring valve replacement, transcatheter aortic valve implantation, or TAVI, is a minimally invasive procedure designed to access the heart through a small incision in the groin. Rather than the traditional open approach of surgical aortic valve replacement (SAVR), which requires patients to recover in hospital up to 7 days, most patients receiving TAVI at the New Brunswick Heart Centre (NBHC) can be discharged next day. However, due in part to the higher upfront procedure cost, there are often barriers to receiving TAVI across Canada, and many health systems have been challenged to find ways to fund this procedure for an increasingly broad base of patients who can benefit from it.

"Fundamentally, the most important reason to augment TAVI in Canada is that these patients do well. They have good short, and long term, proven results,” says Dr. Jean-Francois Légaré, head of cardiac surgery at NBHC.
In 2010, when the NBHC undertook their first TAVI surgeries, it quickly became apparent to them that demand for this procedure would outweigh their allocated budget. By 2016, Dr. Légaré and his team implemented an optimization process in their cardiac care program, focusing on patient needs and benefits. Though the catheter-based TAVI procedure itself is more expensive than SAVR, after weighing reduced length of stay and its ancillary requirements, as well as the improved patient experience, the team at NBHC found novel ways to enable more TAVI procedures within their allocated funding.
“We aim for one day discharge. We don't go to the ICU, we go directly to the floor. We don't intubate patients; we don't put central lines. We streamline our care and minimize all of the invasiveness we can, so there is a lot of cost saving inherent to what we do.”
Using clinical evidence to inform a robust evaluation process over the past 5 years, Légaré and his team also had to consider change management within the hospital establishment. This involved several patient care groups including anesthesia, cardiology, interventional radiologists, nursing, and administration. “Once we were able to demonstrate feasibility, safety, and get the proper education, then the clinical groups were on board, and every staff member on the team was willing to support the changes.”
NBHC is the only primary tertiary care centre for the province and currently performs approximately 150 TAVI cases per year. Most of these cases are done without impacting the regularly scheduled cardiac cath lab cases. The minimally invasive procedure also means cases themselves can be completed in less time than SAVR, which can result in more flexible scheduling for staffing resources.
“We schedule TAVI first in an operating room before the day’s procedures because they can be done within an hour. We can go on with the regular surgical slate in that room without canceling, or delaying, so we’re using the same resources.”
NBHC’s TAVI process hasn’t impacted their ICU capacity, and minimally invasive procedures and other innovative solutions like TAVI may in fact help contribute to reducing pandemic-induced health system wait lists when compared to conventional approaches.
“We have a very strong collaborative program. We can always come to an agreement of what's the best approach for a patient,” says Légaré. “There's no reason to not adapt.”