Stories
Canadian research provides globally relevant affordability model for minimally invasive treatment

How does a more expensive treatment help save healthcare dollars? In a socialized health system, the answer to this question must be supported by robust data. Researchers Derrick Y. Tam, MD, PhD, and Hamid Sadri, PharmD, MSc, MHSc have done just that with their recent study published in the Canadian Journal of Cardiology: Annual Budget Impact Analysis Comparing Self-Expanding Transcatheter and Surgical Aortic Valve Replacement in Low-Risk Aortic Stenosis Patients.*
The authors set out to test a hypothesis regarding the affordability of a minimally invasive treatment with a higher up front procedure cost than its traditional surgical counterpart requiring longer in-hospital recovery. Transcatheter aortic valve replacement (TAVR, also known as TAVI) is a minimally invasive procedure that replaces ailing cardiac valves via a keyhole incision. This contrasts with the less expensive, though more invasive surgical aortic valve replacement (SAVR) option. The latter requires open heart access, which requires longer in-hospital recovery time, and can lead to higher rates of complications.
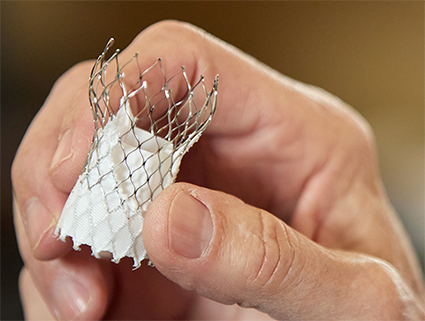
Since its 2012 launch in Canada, physicians have attested to the fact that TAVR delivers better outcomes for patients, while also using fewer hospital resources. Yet the actual cost difference in terms of the full suite of resources was unknown. Tam and Sadri measured associated costs one year out from surgery for both treatments, concluding a total cost difference of approximately 2.8%, feasibly small enough to warrant a shift in budget allocation for cardiac care. They determined that the key difference in cost lays in reduced length of hospital and ICU stay for TAVR, as well as a reduction in adverse events compared to SAVR.
“Rather than focus only on procedural cost, this model demonstrates the advantages of looking outside budget silos to optimize resources as well as patient outcomes,” says study coauthor Hamid Sadri, director of Health Outcomes Research at Medtronic Canada. “This is particularly important as our healthcare system is challenged with human resources constraints after the last few years of pandemic mobilization.”
Previous studies have demonstrated the effectiveness, and feasibility of TAVR, but this is the first to provide a costing model that can be used to show affordability on a global scale. “This cost model helps substantiate evidence-based decisions made at the healthcare management level whether here in Canada, Brazil, or Singapore,” says Sadri. “Health innovation can lead to increasingly complex budgetary decisions, but we now have a model that helps healthcare managers follow the relevant data.”
TAVR, initially developed to treat frail, high-risk AS patients who were unsuitable for the invasiveness of open heart SAVR, has been established as a safe and effective treatment across the risk spectrum for aortic stenosis patients. However, the higher procedural cost of TAVR has led to a perception of unaffordability, which led physicians to prioritize the minimally invasive procedure for higher risk patients. The hope is that this study will help make minimally invasive TAVR more accessible to more patients.